The BCPS remains concerned about access and quality of mental health services for children and youth; so we are continuing to talk to our colleagues at the Ministry of Children and Families, the Ministry of Health and the new Ministry of Mental Health and Addictions.
We know this is an important issue for pediatricians – because we surveyed pediatricians.
According to our 2017 survey of members (of which 162 currently practicing pediatricians responding):
- 75% (122) provide community-based care for patients with mental health disorders (including ADHD, FASD and autism) and/or substance use concerns
Of these 122 pediatricians:
- All provide community-based care for patients with mental health disorders (including ADHD, FASD and autism). They report playing the following roles in the care of these patients:
- Assess and prescribe medication (93%)
- Liaise with school (82%)
- Liaise with other agencies (77%)
- Case management (72%)
- Provide Cognitive Behavioural Therapy (8%)
- Other (8%) – including educating parents, medical management, referral, and administrative
- 42% (51) also provide community-based care for patients with substance use concerns. (All those providing community-based care for patients with substance use concerns also provide care for patients with mental health disorders.)
- One-in-two (53%) report that more than half their practice accounts for patients with mental health disorders or substance use concerns. For 19%, this is three-quarters of their practice or more. An additional 34% report between one-half and three-quarters of their practice is with these patients. A further 47% of these pediatricians report patients with mental health disorders or substance use concerns are less than half of their practice.
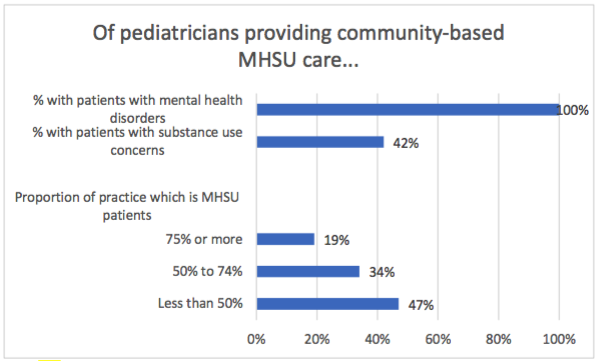
Base: 122 currently practicing pediatricians who provide community-based care for patients with mental health disorders (including ADHD, FASD and autism) and/or substance use concerns responded to the survey
- Only one-in-two (52%) report they have adequate information about agencies/organizations in their community that offer services for child and youth mental health and/or substance use, so that they can appropriately refer.
Of the 162 currently practicing pediatricians who responded to the survey:
- Almost all (93%) have concerns about access to services for their patients with mental health disorders and/or substance use concerns. Their concerns include:
- Timeliness of services (81%)
- Eligibility for available services (60%)
- Location of services (54%)
- Pediatricians outside the Lower Mainland are just as likely as those in other regions to express these access concerns.
Base: 162 currently practicing pediatricians
- Pediatricians have many concerns about the lack of access to services for their patients with mental health disorders or substance use concerns. In particular, they mention concerns about wait times for services, lack of services, crisis management (lack of ongoing support), vulnerability and affordability
Selected Survey Responses:
Extremely difficult to have psychiatrist involved. Referrals to Psychiatry often declined with recommendation that local CYMH office contacted instead. Wait times at CYMH are very long & often psychiatry is not involved or involved in limited capacity.
Most services are private, so many people cannot afford to pay for them. Many Employee Assistance Plans pay only for mental health therapists with whom they have contracts and these therapists are not trained in child and youth therapy. The availability of detox and rehab for SU teens is dismal.
Long term out-patient services in community lag or have fallen so much behind that these pts. End up in getting readmitted frequently to acute care beds in the hospital and wait for days and weeks to be transferred to appropriate psych facility.
Outside lower mainland, there’s limited psychiatry via cymh, almost non-existent psychology (public or even private). CBT isn’t often available, despite evidence that it’s as effective as antidepressants in more mild cases. DBT as well. We’re failing kids with geographical or financial barriers.
Easier to assess one time diagnoses, but very very very hard to get ongoing treatment, such as CBT, or ongoing med management from psychiatry
Vulnerable families have difficulty navigating the system (families who have experienced trauma, have limited literacy, have language barriers). It is difficult to know who best to refer kids to (as a subspecialist)
- Most (70%) are interested in additional training or continuing education related to the treatment of pediatric mental health disorders and/or substance use (this includes those not currently treating MHSU patients as well as those who are). Almost all of these (110 of 113) responding pediatricians are interested in receiving them from the BC Pediatric Society.